Research Areas: Proton Therapy & Immune Response
Lead: Harald Paganetti
Faculty: Ibrahim Chamseddine, Brian Winey, Joost Verburg, Greg Sharp
Postdoctoral Fellows: Nils Peters, Hoyeon Lee, Chris Beekman, Lena Nenoff
Student: Mislav Bobic
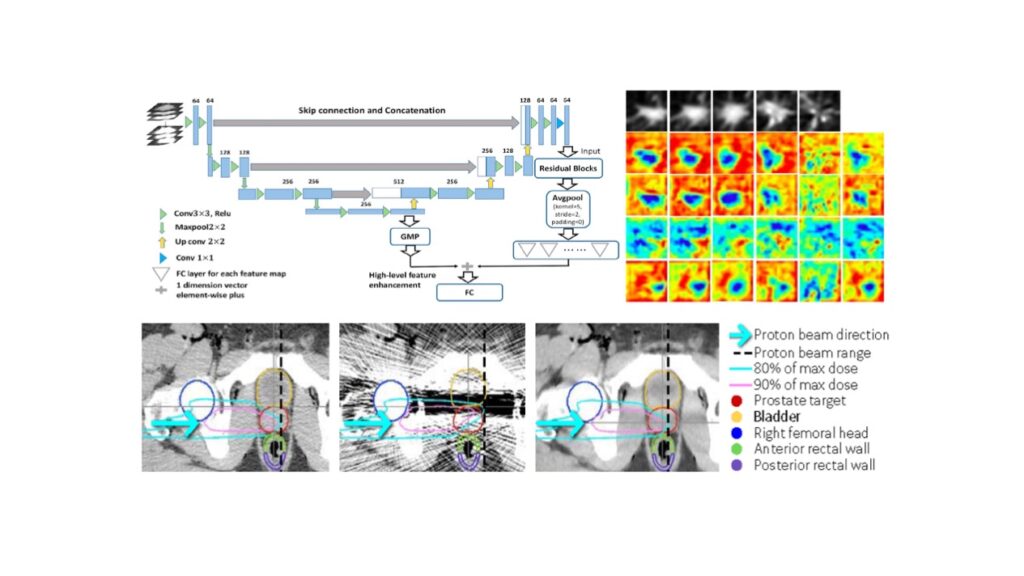
Adaptive Proton Therapy
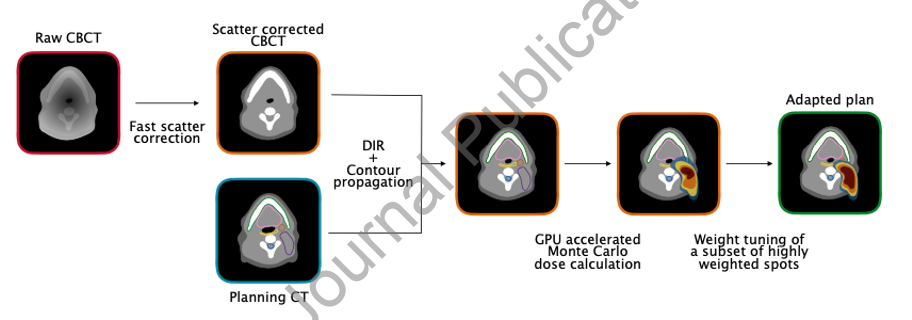
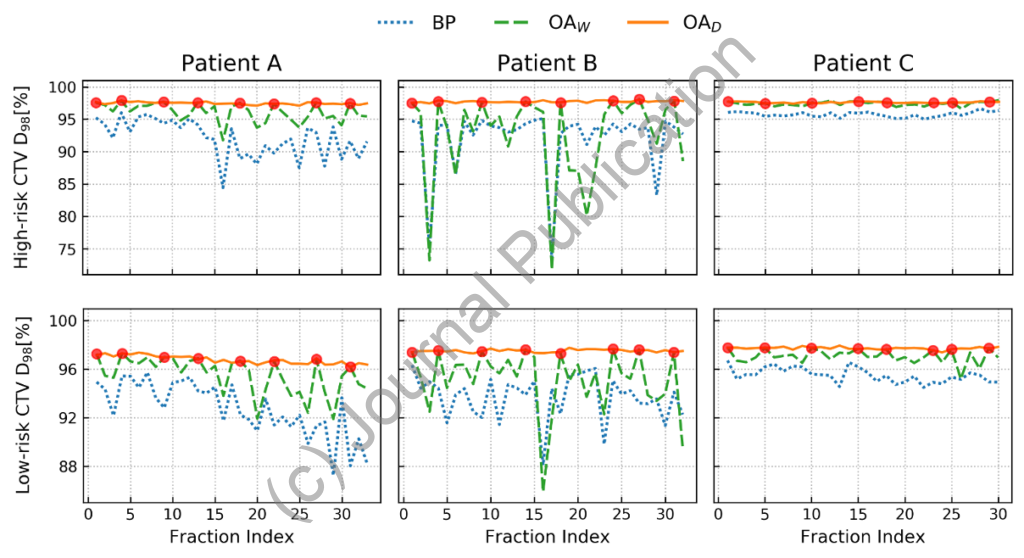
The high conformality of intensity-modulated proton therapy (IMPT) dose distributions causes treatment plans to be sensitive to geometrical changes during the course of a fractionated treatment. This can be addressed using adaptive proton therapy (APT). One important question in APT is the frequency of adaptations performed during a fractionated treatment, which is related to the question whether adaptation has to be done online or offline. The purpose of this work is to investigate the impact of weekly and daily online IMPT plan adaptation on the treatment quality for head and neck patients. A cohort of ten head and neck patients with daily acquired cone-beam CT (CBCT) images was evaluated retrospectively. Dose tracking of the IMPT treatment was performed for three scenarios: base plan with no adaptation (BP), weekly online adaptation (OAW), and daily online adaptation (OAD). Both adaptation schemes used an in-house developed online APT workflow, performing Monte Carlo (MC) for dose calculations on scatter-corrected CBCTs. IMPT plan adaptation was achieved by only tuning the weights of a subset of beamlets, based on deformable image registration from the planning CT to each CBCT. Although OAD mitigated random delivery errors more effectively than OAW on a fraction per fraction basis, both OAW and OAD achieved the clinical goals for all ten patients, while BP failed for six cases. In the high-risk CTV, accumulated values of D98% ranged between 97.15% and 99.73% of the prescription dose for OAD, with a median of 98.07%. For OAW, values between 95.02% and 99.26% were obtained, with a median of 97.61% of the prescription dose. Otherwise, the dose to most organs at risk was similar for all three scenarios. Globally, our results suggest that OAW could be used as an alternative approach to OAD for most patients in order to reduce the clinical workload.
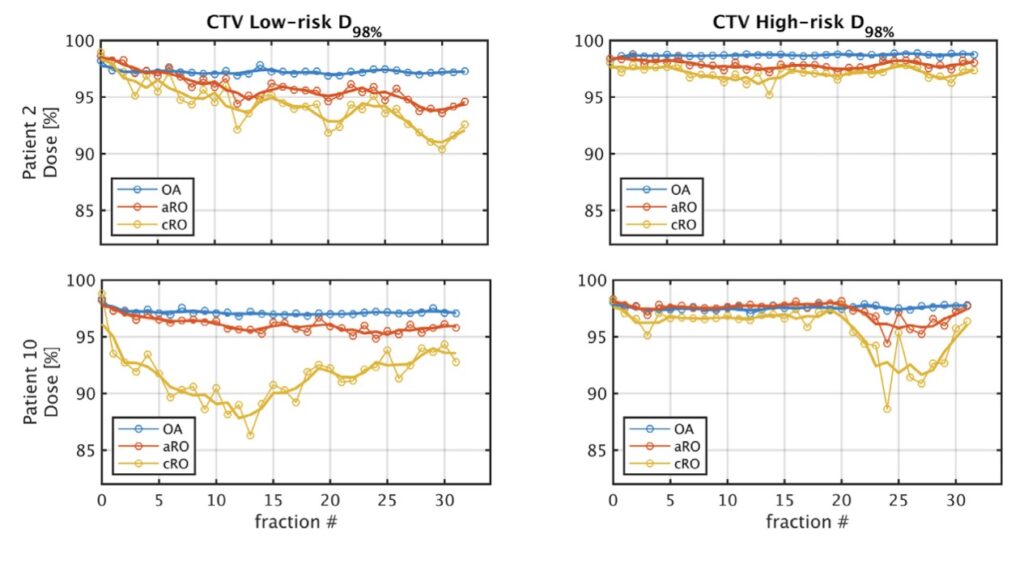
Setup variations and anatomical changes can severely affect the quality of head and neck intensity-modulated proton therapy treatments. The impact of these changes can be alleviated by increasing the plan’s robustness a priori, or by adapting the plan online. The figure shown below compares these approaches. For each patient in the study, three IMPT plans were created: 1- a classical robust optimization (cRO) plan optimized on the planning CT, 2- an anatomical robust optimization (aRO) plan additionally including the two first daily CBCTs and 3- a plan optimized without robustness constraints, but online-adapted (OA) daily, using a constrained spot intensity re-optimization technique only. The cumulative dose following OA fulfilled the clinical objective of both the high-risk and low- risk clinical target volumes (CTV) coverage in all 10 patients, compared to 8 for aRO and 4 for cRO. aRO did not significantly increase the dose to most organs at risk compared to cRO, although the integral dose was higher. OA significantly reduced the integral dose to healthy tissues compared to both robust meth- ods, while providing equivalent or superior target coverage. Using a simple spot intensity re-optimization, daily OA can achieve superior target coverage and lower dose to organs at risk than robust optimization methods.
Metal Artifact Reduction
Risk for developing second cancers in pediatric patients
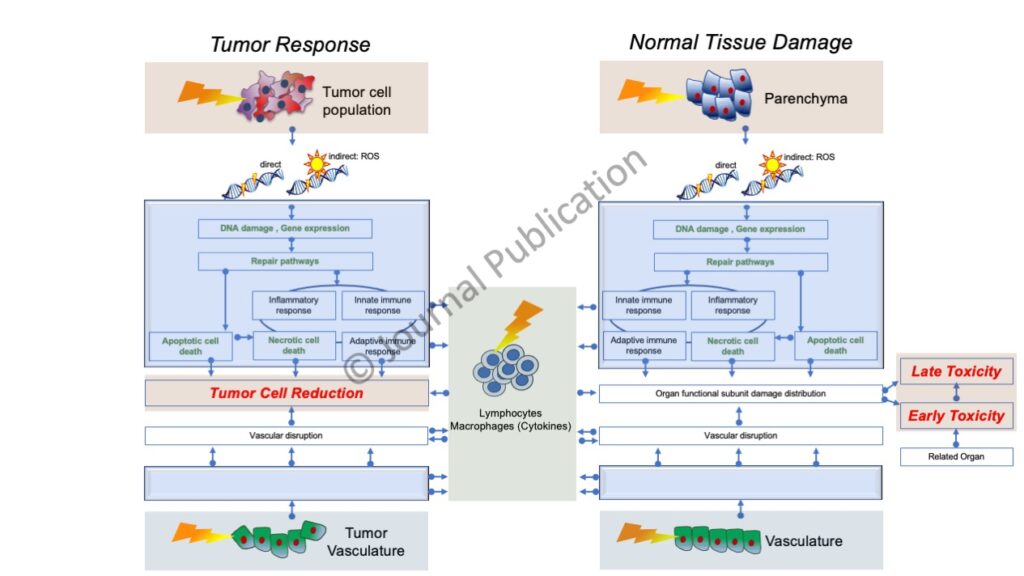
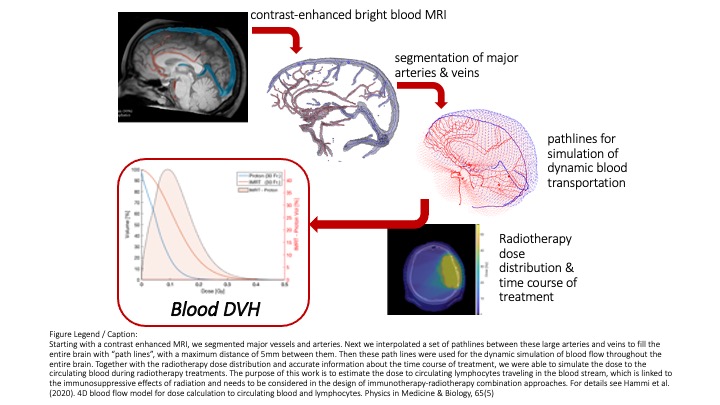
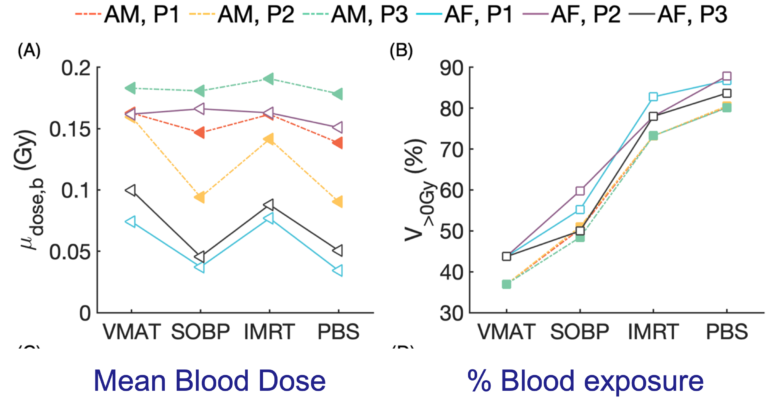
Dose to circulating lymphocytes during radiation therapy
We have developed a time-dependent computational method to estimate dose to circulating blood cells from radiation therapy treatment fields for any treatment site. Two independent dynamic models were implemented: one describing the spatiotemporal distribution of blood particles (BPs) in organs and the second describing the time-dependent radiation field delivery. A whole-body blood flow network based on blood volumes and flow rates from ICRP Publication 89 was simulated to produce the spatiotemporal distribution of BPs in organs across the entire body using a discrete-time Markov process. Constant or time-varying transition probabilities were applied to the Markov process and their impact on transition time was investigated. Applying this framework, the impact of treatment time and anatomical site were investigated using imaging data and dose distributions from a liver cancer and a brain cancer patient. The impact on the blood dose-volume histograms (bDVHs) was assessed using bDVH metrics (V0Gy, V0.125Gy, V0.5Gy, D2%). The simulations revealed different dose levels to the circulating blood for brain irradiation compared to liver irradiation even for similar field sizes due to the different blood flow properties of the two organs. The volume of blood receiving any dose (V0Gy) after a single radiation fraction increases from 1.2% for a 1-second delivery time to 20.9% for 120-second delivery time for the brain cancer treatment, and from 10% (1s) to 48.7% (120s) for a liver cancer treatment. Other measures of the low-dose bath to the circulating blood such as the dose to small volumes of blood (D2%) decreases with longer delivery time. Furthermore, we demonstrate that the bDVH is highly sensitive to changes in the treatment time, indicating that dynamic modeling of blood flow and radiation fields is necessary to evaluate dose to circulating blood cells for the assessment of radiation induced lymphopenia. The developed framework is publicly available and allows for the estimation of patient-specific dose to circulating blood cells based on organ DVHs, thus enabling the study of the impact of different treatment plans, dose rates, and fractionation schemes.
Proton RBE